After 1975
Depression in the Elderly Population of the Vietnamese Community in Orange County, California Part 2/3
Published on

Editor’s Note: This work was written by Huyen Duc Duong and originally edited by Duong Nhu Nguyen and Nhu Duc Dzuong. For readability, the study has been edited for style and is published as a three-part series. For the purpose of furthering academic inquiry, the US-Vietnam Review will publish works such as the following, however, please be advised that the Review does not endorse all contextual interpretation herein.
PART II: REVIEW OF THE RELEVANT LITERATURE
A. Prevalence of depression in relation to ethnicity
The following data were found as of 2008, the timing of the case study made the subject of this paper.
Estimates on the prevalence of depression among the older population varied from 10 percent up to 65 percent (see www.psychinstitute.com/mental_illness/depression_in_elderly. html). The reason for this wide range was that many of those who have the disorder were often misdiagnosed. Many older individuals who suffered from depression were not diagnosed at all. Many accepted their symptoms as an inevitable part of aging, and hence sought no help. Others viewed their feeling downhearted as shameful. Another prevalent concern in the elderly population was their generational resistance to the idea of emotional illness, and their doubt toward the benefits of seeking professional help.
The following conclusions are still valid today as was at the time of the case study, because they are based on cultural observations that have not changed since 2008.
Asian American elders, for example, attach a strong stigma to any form of mental illness, resulting in either underdiagnosis or simply overlooking or ignoring the possibility of depression (Surgeon General, 200l). Many senior citizens are sufficiently embarrassed by what they consider to be the stigma caused by their symptoms, such that they are unwilling or unable to discuss their feelings with others. A large number of them are also discouraged from seeking treatment because of financial constraints.
Yet, because treatment for depression can dramatically improve the quality of these later years, a correct diagnosis and professional attention are extremely vital. Kinike Bennuder, Consumer At the beginning of the millennium, the Program Director for the MHA of Greater Dallas and a spokesperson for Asians and Pacific Islanders, noted that 40 percent of Asian refugees suffer from depression, 35 percent from anxiety, and 14 percent from PTSD (Post Traumatic Stress Disorder). By comparison, at the beginning of the century, the Spanish population in the U.S. numbered 36 million, a 700 percent increase in 40 years, but of these 36 million, one third were uninsured, half did not have personal physicians, and about 30 percent of this immigrant population were depressed.
It has been observed that elderly Hispanic and African Americans have higher rates of depression than their white counterparts, due largely to greater health burdens and lack of health insurance, a Northwestern University study has found. As of 2008, the study, published in an online issue of the American Journal of Public Health, showed that major depression was most prevalent among Hispanic – 10.8 percent — followed by almost 9 percent in African Americans and approximately 8 percent in whites in the same age group.
The odds of depressive disorders among older Hispanics showed 44 percent greater than among whites, representing a significantly greater prevalence of major depression, said lead author Dorothy D. Dunlop, research associate professor at the Institute for Health Services Research and Policy Studies at the Feinberg School of Medicine at Northwestern University.
At the beginning of the millennium, more than two million of the 34 million Americans age 65 and older suffered from some form of depression (National Institute of Mental Health, 1999). Of the nearly 35 million Americans — 65 and older, an estimated 2 million have a depressive illness, and another 5 million might have depressive symptoms, according to official federal health estimates.
According to the 2001 Surgeon General’s report on mental health, the prevalence of mental disorders was believed to be higher among African-Americans than among whites, and African-Americans were more likely than whites to use the emergency room for mental health problems. African-Americans with depression were less likely to receive treatment than whites (16 percent compared to 24 percent). Only 26 percent of African-Americans with diagnosed generalized anxiety disorder received treatment for their disorder, compared with 39 percent of whites with a similar diagnosis.
It was no surprise that a large number of Southeast Asian refugees suffered from mental health concerns resulting from their refugee experience: their sudden and involuntary cultural transplantation to a foreign culture, in the name of freedom. Researchers focusing on this group recognized that the older refugees had spent many years in squalid refugee camps, and many had been held in political-detainee prisons in Vietnam for a decade or more (Mollica, Mcinnes, Phan, et al., 1998). In addition to the trials and tribulations of acculturation and adaptation to Western life, numerous stressors prior, during, and after refugee migration, plus horrific life-events during the Vietnam War and its aftermath, all justifiably led to depression as a result of irreparable losses and post-traumatic stress syndrome. As early as the 1980 and throughout the 1990s, it was already recognized in research studies that Southeast Asian elderlies appeared to suffer from a higher risk of psychological distress than younger Southeast Asians, because the older generation had fewer buffers and coping strategies to deal with their distress (Shapiro, et al., 1999; Yee, 1997; Yee & Thu, 1987).
Specifically, a small community study of Vietnamese immigrants in Boston found the following: 32% smoked (54% males, 9% females); 24% used alcohol; 17% were depressed on a carefully constructed “Vietnamese Depression Scale,” with those older than 40 having more depression symptoms than younger ones (Nelson, Bui, & Samet, 1997). Likewise, an exploratory study conducted by Tuyen D. Nguyen, Susan Larsen, Brian Lam & Toan Phan (2006) found that Vietnamese elderly immigrants were identified as clinically depressed — as much as 21% of the 200 sampled elderly Vietnamese immigrants residing in Orange County, California.
Tragically, the depressed elderlies were more likely to take their own lives. Comprising just 13 percent of the U.S. population, people age 65 and older accounted for 18 percent of all suicides in 2000, according to the National Institute of Mental Health.
B. Causes of Depression
Pathophysiologic theories of affective disorders have developed along three major lines:
- endocrine studies; (2) neurotransmitters; and (3) electrophysiologic studies. Findings
include:
–Depressed patients frequently have elevated levels of cortical steroids in the blood and urine, and at least half of the studied population fail to suppress cortisol secretion after dexamethasone administration.
–TSH response to thyrotropine-releasing hormone also has been found to be aberrant in many depressed patients, even though their blood T3 and T4 levels are normal. Growth hormone, prolactin, gonadal hormones, corticotrophin-releasing factor, and melatonin have all been shown to have diminished responses in subgroups of affective disorders.
Although none of these findings is specific for any type of depressive illness or consistent in all depressive illnesses, they nevertheless suggest the presence of pituitary-hypothalamic dysfunction in affective disorders (Bennett & Plum 1996).
–It has been believed that depression is a biologically heterogeneous disorder; that is, many central nervous system (CNS) neurotransmitter abnormalities can cause clinical depression (Delgado et al,1992). The two main neurotransmitters are serotonin and norepinephrine.
–Electrophysiologic studies on affective illnesses have concentrated on changes in sleep functions, especially the presence of changes in the REM sleep pattern during episodes of active illness. A subgroup of patients with affective disorders shows a shortened REM latency (Bennett & Plum, 1996).
–Medical conditions: Certain medical problems, such as hormonal imbalance, nutritional deficiencies, heart disease, and certain cancers can physically create the symptoms of depression.
–Medications for illnesses, particularly high blood pressure or arthritis, can cause drug interaction leading to depressive symptoms and mood changes.
C. Signs and Symptoms of Depression
As already pointed out, many elders who have depression are not diagnosed at all. Acceptance of symptoms as an inevitable part of aging means that no help is sought. Generational resistance to the idea of emotional illness, not recognizing the benefits of seeking help, embarrassment, subjective view of stigmatization, and shame psychology also contribute to the lack of diagnosis and accurate data. The problem perpetuates itself because of failure to recognize the need for talking therapy. Depression can particularly be hard to recognize in the elderly population because some of its more insidious symptoms (such as fatigue, loss of appetite, and disrupted sleep pattern) can also be caused by, and are often blamed on, other physical illnesses.
Yet, depression is more than an occasional feeling of sadness or a natural, grieving response to loss. It is a group of long-lasting or recurring emotions and behaviors that interfere with a person’s normal activities. Generally, a diagnosis is based on whether someone has experienced four or more of the following symptoms continually or most of the time for more than two weeks:
- Depressed mood most of the day, as indicated by either subjective report (e., feeling sad or empty) or observation made by others (e.g., appears tearful).
- Markedly diminished interest or pleasure in all, or almost all, activities most of the day, nearly every day (as indicated by either subjective account or observation made by others).
- Significant weight loss or weight gain when not dieting (e., more than 5% of body weight in a month), or decrease or increase in appetite nearly every day.
- Insomnia or hypersomnia nearly every
- Psychomotor agitation or retardation nearly every day (observable by others, not merely subjective feelings of restlessness or being slowed down).
- Fatigue or loss of energy nearly every
- Feelings of worthlessness or excessive or inappropriate guilt (which may be delusional) nearly every day (not merely self-reproach or guilt about being sick).
- Diminished ability to think or concentrate, or indecisiveness, nearly every day (either by subjective account or as observed by others).
- Recurrent thoughts of death (not just fear of dying), recurrent suicidal ideation without a specific plan, or a suicide attempt or a specific plan for committing suicide (Bennett and Plum, 1996).
For many victims of depression, these mental and physical feelings seem to follow them night and day, appear to have no end, and are not alleviated by happy events or good news. Some people are so disabled by feelings of despair that they cannot even build up the energy to call a doctor, or they may refuse to go because they are so hopeless that they think there is no point in seeing a professional.
The diagnosis of an affective disorder is made on clinical grounds as discussed above.
Many tests to aid the diagnosis of depression have been introduced, including the dexamethasone suppression test (DST), the thyroid-stimulating hormone (TSH) response, and many measures of disturbed sleep function such as rapid eye movement (REM) latency. Unfortunately, none has proved to be diagnostically reliable or specific for affective disorders. ln diagnosing depression, the interview is central (Bennett and Plum, 1996).
D. Depression Treatment
Most people with depression can get effective help from treatment. For many, spotting depression early and getting treatment might cut down on how long and how serious the depression can become. The following description is based on what has been used in the medical profession.
Depression Treatment Options
The most common treatments are antidepressant medicines, “talk” therapy, or a combination of both. The sufferer and his or her doctor can work together to decide on the right depression treatment.
- Medication
Studies show that antidepressants have been effective in treating depression. A type of medicine called selective serotonin reuptake inhibitors (SSRIs) is most often prescribed by doctors.
- Psychotherapy
ln “talk” therapy, the patient and therapist talk about the patient’s experiences, relationships, events, and feelings. Two of the approaches found to be effective for treating depression are interpersonal therapy and cognitive-behavioral therapy (CBT).
- Interpersonal therapy
Interpersonal psychotherapy is a short-term psychological treatment for depression. It focuses on the role of the dysfunctional interpersonal relationships at the onset and during the perpetuation of depression (Elizabeth 1998). This approach looks at the patient’s personal relationships that both cause depression and make it worse.
- Cognitive-Behavior therapy (CBT)
The use of specific cognitive interventions has proved successful in individual therapy with depressed persons. Cognitive therapy for depression is brief, structured, and directive treatment designed to alter dysfunctional beliefs and depressive patterns (Haaga and Beck, 1992).
Essentially, the depressed person learns:
- The connection between thoughts and feelings
- The negative thought pattern typical of depression
- How different feelings can emerge when the sufferer is taught to alter his thinking under the same
Behavioral therapy has gained data and proven outcome from both people and the environment in which they function. Behavioral therapy also attempts to decrease the number of negative interactions between patients and others coming into contact with them (Elizabeth, 1998). Talking about the difficult areas of life and trying to work them out is very valuable and can reveal some, if not all, of the root causes behind depression. Working with a caring therapist can help patients find better ways of dealing with their problems.
Phases of Depression Treatment with Medication and Psychotherapy
There are three phases of depression treatment:
- Treatment phase 1: Acute Phase
During the acute phase, the person starts taking medication. Hopefully, the symptoms of depression become less severe, and the person begins to feel better. If moderate improvement is not seen in the following 6 to 8 weeks after starting medication, treatment might need to be adjusted. This phase lasts for the first 6 to 16 weeks, during which the patient takes an antidepressant.
- Treatment phase 2: Continuation Phase
During this phase, the person continues to take medication to prevent depression symptoms from corning back. This phase lasts from 6 to 20 weeks after the symptoms first subside. In general, the person will keep taking depression medication at the same dosage during this phase. The person should not stop taking an antidepressant without talking to a doctor.
- Treatment phase 3: Maintenance Phase
The purpose of this phase is to prevent another episode of depression. In this phase, treatment that was effective during the acute and continuations phase should be used. How long this phase lasts depends on the person’s medical history and on the advice of a doctor or other qualified healthcare professionals.
(see www.zoloft.com/zoloft/zoloft.p01ial? Nfpb=true& pagelabel=learning about depression).
3) Electroconvulsive Therapy (ECT)
Electroconvulsive therapy may be indicated when antidepressant drugs have no effect; however, in some situations, ECT may be considered a primary treatment and may be given before a trial of antidepressant medication. ECT is indicated when (Dubovsky, 1995):
- There is a need for a rapid, definitive response when a client is suicidal or
- A client is in extreme agitation or
- The risks of other treatments outweigh the risks of
- The client has a history of poor drug response, a history of good ECT response, or
- The client prefers
The controversial nature of ECT makes this area sensitive for generalized discussion, and should be a separate topic for the clinical community.
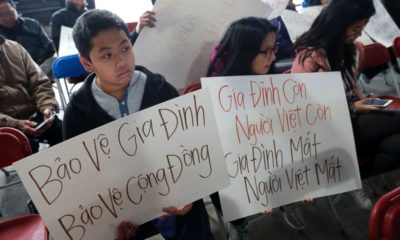
C. Treatment of Southeast Asian American Depressed Elderlies
As already discussed above, massive immigration of Southeast Asians to the United States began primarily after the communist takeover of Cambodia and Vietnam in 1975. Although immigration was voluntary, Vietnamese refugees were actually driven from their homeland by regional strife, often leaving behind family members. The first wave of Vietnamese refugees – those arriving prior to 1978 – typically had contact with American servicemen or civilians during the Vietnam War. While many left empty-handed and under heartbreaking conditions, there were the privileged few who brought with them not only education but also economic resources. Generally, the journey, where sponsored and organized by the U.S., was fairly safe.
Those who came later were more likely to have fled the communist regime under dire circumstances. Typically, many latecomers were from rural areas and tended to be less westernized, less educated, and less equipped to adapt to a highly technological society such as the U.S.
Vietnamese elders, most of whom accompanied their children to the U.S., in many cases had to depend on their children and grandchildren for negotiating with their new American environment. Dramatic role reversals in the family that produced negative effect on mental health should be analyzed and understood in the following contexts:
- Economic situation
Where the older generation could obtain employment in their new surroundings, the median income of Vietnamese elderly men and women was substantially less than that of AngloAmerican elderlies. The reasons for this gap were obvious: limited English ability, inadequate education, discrimination in hiring and rates of pay, work histories of low-wage jobs, and high unemployment resulting in lower Social Security and private pension plan coverage (Manuel, 1982).
- Health
The mean life expectancy of Asian Americans is higher than for the Anglo-Arne1ican population. However, despite their greater longevity, Asian American elderlies are more likely to have debilitating health problems than their Anglo-American peers. Much of this differential in health status can be attributed to lower income levels among Asian Americans, lack of adequate health care throughout life, and a greater likelihood of working at manual, physically debilitating jobs. Moreover, health care service utilization by Asian American elderlies is restricted because of language difficulties, preference for traditional Eastern folk medicine, distrust of services from the dominant culture that has historically discriminated against them, reduced eligibility for Medicare because of work histories, and an unwillingness to use Medicaid because it is perceived as a sign of stigmatizing poverty or inability to take care of oneself.
A smaller percentage of Asian-Americans (3%) compared to Anglo elderlies (5.8%) live in nursing homes. Among the oldest of the elderly population, only I 0% of Asian-Americans and Pacific Islanders are institutionalized for old-age caregiving, as compared to 23% of Anglo-Americans. Reasons for this difference include discrimination in referrals to long-term care services, potential linguistic isolation, geographical discrimination in nursing homes, and greater involvement of families and other unpaid sources of assistance for Asian Americans (Manual, 1982). In addition, Asian American and Pacific Islander groups place a high value on caring for elderly members within the family, and attach a social stigma to institutionalization.
- Family
Asian cultures traditionally emphasize the primary role of family bonds and unquestioned respect for elderly family members, although this trend has decreased due to impact of the mainstream culture upon newer generations of Asian Americans. For most Asian Americans and Pacific Islanders, the family performed a crucial function in the immigrants’ new surroundings, providing a haven from a racist society and an environment where self-esteem “the Asian way” could be developed and creative coping tactics promoted. (However, many Asian Americans deny encounters with racism out of their cultural pride – discrimination to them may mean they cannot overcome challenges in the new environment, cannot adapt, and cannot win the respect of the natives.)
Many traditional Asian practices and beliefs regarding family interaction and concepts of self-worth are based on Confucian philosophy, which asserts the importance of social order within families and society, nurturing a noble sense of self-respect, self-containment, and self-sacrifice for the higher good. Roles, responsibilities, and status in the family are prescribed by elderlies, and transcend personal desires or bonds based on outward expression of affection. Loyalty to the family is a longterm commitment and is maintained through a system of obligations that must be repaid by younger family members who owe their filial piety to their elderlies. The elders in traditional Asian families are the authority figures, who control family’s finances and have the final say over decisions affecting the lives of younger family members. Asian American and Pacific Islander families often face conflict between these traditional values and the popular culture of the United States, which tends to value individualism, independence, autonomy, and youth. When Americanized Asian family members no longer abide by prescribed roles, duties, and responsibilities of their traditional culture, elderly members find themselves no longer having control over family financial resources and decision-making, many times experiencing the shame of becoming dependent upon children and grandchildren for support and for negotiation in the new, unfamiliar environment. ln addition, their Americanized children look up to the dominant society and, with their upward mobility, are often required to relocate for employment, thereby altering the traditional pattern of family support (Kii, 1984).
- Social Relationship and Communal Involvement
Strong peer and communal support systems are important resources that Asian American and Pacific Islander elders rely on as they approach their later years. As a result of impoverished circumstances and racial discrimination, in time of needs, immigrants are forced to rely heavily upon their ethnic peer, family and informal communal support systems. Assistance from the majority cultural institutions typically is not available to them, and hence, economic, emotional and social support is found primarily within ethnic enclaves. These enclaves often are the only environment where the monolingual immigrant can function. There, most social relationships develop and cultural institutions such as community-specific churches and peer groups can flourish. In addition, ethnic-specific service centers and NGOs or social service agencies can also develop, often based on local, state, and/or federal fundings to serve the needs of ethnic immigrants and elderlies who are concentrated in these enclaves, but that does not necessarily mean these funded agencies can meet the needs. Shame and self-consciousness, as well as the psychology of pride, would keep the elderlies from seeking help or receiving what they consider as “charity.” These reservations are gradually disappearing, as Asian immigrants recognize the culture of practicality that characterizes businesses and entrepreneurial America: whatever works to the advantage of the recipients is now the morale. However, more recent immigrants have not had the opportunity to develop an adequate support network, and the community self-help enclaves of support groups have dwindled down due to decreased membership. Nor do newly arrived immigrants have sufficient English skills to interact outside their ethnic enclaves or with the younger generations that become the leadership of the funded agencies. The elderlies generally cannot drive, and therefore may be isolated from regular contact with the friends they have made from their enclaves. It has been founded that more than 85% of Southeast Asian American elders live with their families, among younger family members who provide for almost all of their economic and social support. As already stated earlier, such extensive dependence on younger family members reverses the traditional family roles, thereby exacerbating the difficulties of adapting to the new environment and the challenges faced by both generations.
About the author & Editors
Dr. Huyen Duc Duong, M.D., M.S., graduated from the University of Saigon, Faculty of Medicine, in 1972. After 1975, he also researched and practiced Acupuncture and Eastern Alternative Medicine, in addition to family practice and internal medicine. In America, he received graduate training as a gerontologist at California State University in Fullerton. A martial art practitioner and trainer (Aikido and Tai Chi), he holds a golden second belt in Vovinam, the official martial art of Vietnam.
Dr. Nhu Duc Dzuong, B.A., M.A, Ph.D. (deceased): A British Council and Fulbright Scholar, Dr. Dzuong was trained in linguistics at the University of London’s University College and the School of Oriental and African Studies, England. In America, he specialized in bilingual education and educational leadership. From 1966 to 1967, he was Deputy for the Minister of Culture and Education (Công Cán Ủy Viên Bộ Giáo Dục), representing Minister Tran Ngoc Ninh at ASEAN and in the U.S. for the study of Social Security and Medicare, with the goal to adapt these two systems to the RVN.
A Fulbright Scholar, Ms. W. Nhu-Nguyen Duong, B.S., J.D., LLM, is a published author of literary novels, cultural essays, and law or interdisciplinary reviews. She is a lawyer, former judge, and former law professor. She also holds interests and received training in journalism, drama, psychology, and music.
You may like
-


“The Common Place of Law” in the “Uncommon” World of Vietnamese Immigrants: The Vietnam War Refought in Massachusetts
-


Striving for a Lasting Peace The Paris Accords and Aftermath
-

Love Found and Lost: The Kim Vui’s Story (Book Review)
-


Upcoming Event: 5/10/23 Hidden Histories: The South Vietnamese Side of the Vietnam War
-


Depression in the Elderly Population of the Vietnamese Community in Orange County, California Part 3/3
-

Nam Phong Dialogues: Episode 14 Vietnamese Anticommunism

Reflections on New Era of National Rise by Vietnam General Secretary Tô Lâm

Of Space & Place: On the Nationalism(s) of Tuan Andrew Nguyen’s “Our Ghosts Live in the Future”

Postwar Music In Vietnam And The Diaspora

Translation: The Decision in 2013 of the Central Committee of the Communist Party of China on Certain Major Issues Concerning Comprehensively Deepening Reform

Thủ Đức Demonstration High School: A Modern Educational Policy and Teaching Method of the Republic of Vietnam

Vietnam’s unresolved leadership question

Rethinking History and News Media in South Vietnam

“The Vietnam War Was an Unwinnable War”: On Factuality and Orthodoxy

Pandemics and Morality: Lessons from Hanoi

Democracy in action: The 1970 Senatorial elections in the Republic of Vietnam (Part 1)
US-VIETNAM REVIEW
-

 Politics & Economy4 years ago
Politics & Economy4 years agoVietnam’s unresolved leadership question
-

 Politics & Economy2 years ago
Politics & Economy2 years agoRethinking History and News Media in South Vietnam
-

 After 19751 year ago
After 19751 year ago“The Vietnam War Was an Unwinnable War”: On Factuality and Orthodoxy
-

 Society & Culture5 years ago
Society & Culture5 years agoPandemics and Morality: Lessons from Hanoi
-

 ARCHIVES5 years ago
ARCHIVES5 years agoDemocracy in action: The 1970 Senatorial elections in the Republic of Vietnam (Part 1)
-

 Politics & Economy4 years ago
Politics & Economy4 years agoThe Limit to U.S.-Vietnam Security Cooperation
-

 Politics & Economy5 years ago
Politics & Economy5 years agoNational Shame: How We (Americans) can learn from Nguyễn An Ninh
-
 Vietnamese-America4 years ago
Vietnamese-America4 years agoDeporting Vietnamese Refugees: Politics and Policy from Bush to Biden (Part 1)

